Varicose Veins: Causes, Symptoms, and Treatment Options
I. Introduction
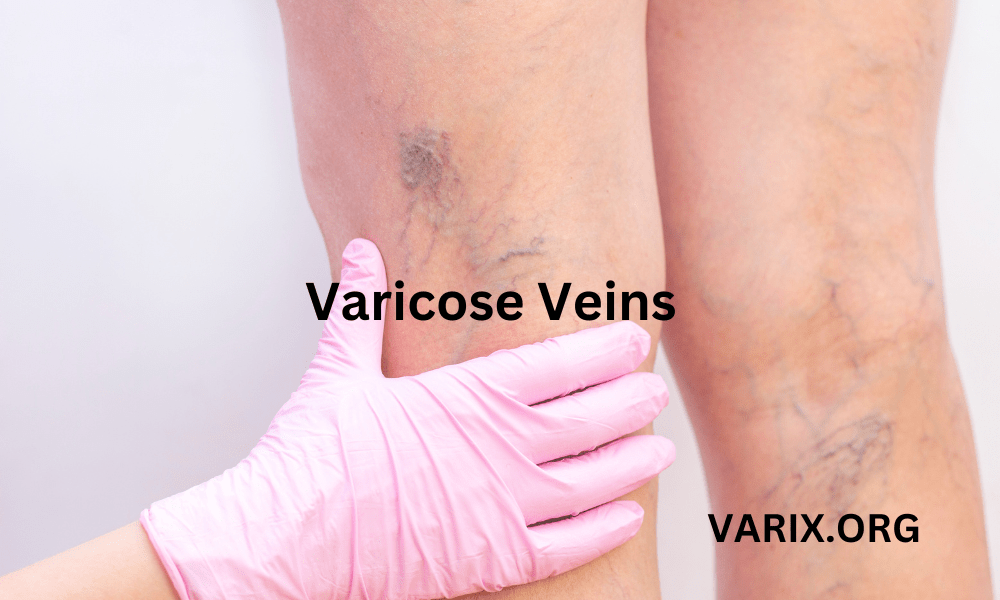
A. Brief Overview of Varicose Veins
Varicose veins are enlarged, swollen, and twisted veins that most often appear blue or dark purple. They develop when the one-way valves in veins become weak or damaged, allowing blood to flow backward and pool in the vein. This pooling causes the vein wall to stretch and bulge. While varicose veins can occur anywhere, they typically arise in the legs and feet because standing and walking increase pressure in those veins. Beyond appearance, varicose veins may cause discomfort, pain, heaviness, and itching. In advanced cases, they can lead to complications such as skin changes, ulcers, or blood clots.
B. Importance of Understanding Varicose Veins
With millions affected worldwide, varicose veins represent a significant public health concern. Although not always life-threatening, they can negatively impact quality of life, self-esteem, and mobility. Early recognition of symptoms and risk factors enables individuals to seek timely intervention, reducing the likelihood of severe complications. By learning why varicose veins form and how to manage them, you can take proactive steps—such as adopting healthier habits and exploring treatment options—to maintain optimal vascular health and prevent future problems.
II. What Are Varicose Veins?
A. Definition and Description of Varicose Veins
Varicose veins are superficial veins that become enlarged, twisted, and visible beneath the skin’s surface. Healthy veins contain one-way valves that open to allow blood to flow toward the heart and close to prevent backflow. When these valves weaken or fail, blood can pool in a segment of the vein. Over time, persistent pooling stretches the vein, causing it to appear swollen, knotted, or rope-like. The skin overlying the vein may become thin or discolored, and the vein itself often turns a bluish or dark purple hue.
B. Varicose Veins vs. Spider Veins
Varicose veins and spider veins (telangiectasias) both result from venous insufficiency, but they differ in appearance, size, and severity. Spider veins are smaller, red or blue, thread-like veins that lie closer to the skin’s surface and often appear in web-like patterns. They typically cause minimal discomfort and are primarily a cosmetic concern. Varicose veins, on the other hand, are larger, bulging veins that carry a higher risk of symptoms and complications. Individuals may have both conditions simultaneously, but treatment strategies differ based on vein size and symptom severity.
C. Varicose Veins in Different Body Areas
1. Legs
The calf and thigh veins are the most common sites for varicose veins. Gravity places extra pressure on leg veins, and the valves in these veins are under constant strain to push blood upward. Risk factors related to leg varicosities include prolonged standing or sitting, obesity, pregnancy, and genetic predisposition.
2. Feet
Varicose veins can form on the feet when venous pressure increases and vein walls weaken. Symptoms on the feet mirror those in the legs: swelling, aching, and discomfort, especially after extended periods of standing. Foot varicosities often accompany leg vein disease and may require comprehensive evaluation.
3. Testicles (Varicocele)
A varicocele is a varicose vein in the scrotum, affecting the pampiniform plexus of veins. It is common in males aged 15–25 and can contribute to discomfort, a feeling of heaviness, and fertility issues. Affected men may experience a dragging sensation in the scrotum or notice a soft, bag-like mass above the testicle. Treatment options range from conservative measures to surgical repair, depending on severity and impact on fertility.
4. Vulvar and Vaginal Varicose Veins
Hormonal fluctuations and increased pelvic blood flow during pregnancy can cause varicose veins in the vulvar or vaginal area. Although these varicosities often resolve after childbirth, some women continue to experience discomfort—itching, aching, or a feeling of fullness— postpartum. If symptoms persist, interventions such as compression or sclerotherapy may be considered to provide relief.
III. Causes of Varicose Veins
A. Risk Factors and Common Causes
Varicose veins arise when vein valves weaken or fail, preventing proper blood flow back to the heart. Over time, pooled blood stretches vein walls, resulting in enlarged, bulging veins. Common contributors include:
- Age: Aging reduces vein wall elasticity and weakens valves, increasing the risk of valvular failure.
- Genetics: Family history significantly influences vein valve strength and vein wall resilience. If parents or siblings have varicose veins, your risk is higher.
- Obesity: Excess body weight adds pressure on leg veins, making it harder for valves to function properly and causing blood to pool.
- Prolonged Standing or Sitting: Jobs or lifestyles involving long hours seated or on your feet slow circulation. When muscles do not contract regularly, blood can collect in leg veins.
- Gender and Hormones: Women are more likely to develop varicose veins due to hormonal influences from menstrual cycles, pregnancy, and menopause. Estrogen and progesterone can relax vein walls, making valves more prone to failure.
B. Varicose Veins During Pregnancy
Pregnancy increases the risk of varicose veins because blood volume expands to nourish the fetus, placing additional stress on vein walls. Hormonal changes relax vein walls, and the growing uterus exerts pressure on pelvic veins, further impeding blood return from the legs. Varicose veins that develop during pregnancy often improve after childbirth, but persistent cases may require medical evaluation and conservative management—such as wearing compression garments and elevating the legs—to ease discomfort until veins return to normal.
C. Varicose Veins in One Leg Only
Occasionally, varicose veins affect only one leg. This can occur if a local issue—such as a blood clot (deep vein thrombosis), previous vein injury, or post-surgical damage—compromises valve function in that leg. When varicose veins appear unilaterally, it is crucial to seek evaluation to rule out underlying vascular conditions. Duplex ultrasound can assess blood flow and valve competence in both legs to determine the root cause.
Recognizing the causes and risk factors for varicose veins empowers you to take preventive steps. Early intervention—through lifestyle changes or medical treatments—can reduce discomfort, slow progression, and minimize the risk of complications.
IV. Symptoms of Varicose Veins
A. Early-Stage Symptoms
In initial stages, varicose veins may appear as visible, bulging veins without causing any discomfort. As vein pressure increases and inflammation develops, you may notice:
- Aching, throbbing, or cramping in the legs
- Heaviness or fatigue in legs after standing or walking
- Itching or burning sensation around affected veins
- Swelling in ankles, feet, or lower legs that worsens over the day
- Restless leg sensations at night disrupting sleep
B. Advanced Symptoms and Complications
If varicose veins persist without intervention, more severe symptoms and complications may arise:
- Skin Discoloration: Brownish or reddish patches (stasis dermatitis) appear near ankles.
- Lipodermatosclerosis: The skin over affected veins may harden, thicken, or become tender.
- Venous Ulcers: Painful, slow-healing sores usually develop near the ankles; they can leak fluid and are prone to infection.
- Bleeding: Veins close to the skin surface may rupture with minor trauma, causing bleeding that requires prompt medical care.
- Superficial Thrombophlebitis: A clot in a superficial vein can cause localized pain, redness, warmth, and tenderness along the vein’s course.
- Deep Vein Thrombosis (DVT): Though rare, varicose veins increase the risk of clots in deeper veins. Symptoms include sudden calf or thigh pain, significant swelling, redness, and warmth, potentially leading to life-threatening pulmonary embolism if untreated.
Prompt recognition of advanced symptoms and complications is essential. If you notice skin changes, persistent pain, swelling, or signs of a blood clot, seek professional evaluation immediately. Timely diagnosis and intervention can prevent serious outcomes.
V. Prevention and Self-Care for Varicose Veins
A. Compression Stockings and Socks
Graduated compression stockings apply the greatest pressure at the ankle, gradually decreasing up the leg. This gradient of pressure promotes blood flow back toward the heart, reducing pooling in the lower legs, alleviating swelling, and minimizing discomfort. Key points:
- Choose the correct compression level: 15–20 mmHg for mild symptoms, 20–30 mmHg for moderate pain or post-treatment support, and 30–40 mmHg for severe cases under professional guidance.
- Ensure proper fit: Measure ankle, calf, and, if needed, thigh circumference to select the right size. Many clinics offer professional fitting services.
- Wear daily: Put on stockings in the morning before swelling begins and remove them at night.
- Replace regularly: Compression garments lose elasticity after three to six months of daily use, so replace them to maintain effectiveness.
B. Lifestyle Changes
Adopting healthy habits can slow varicose vein progression and improve overall vascular health:
- Regular Exercise: Low-impact activities—walking, swimming, and cycling—strengthen calf muscles and boost venous return. Aim for at least 30 minutes of moderate exercise most days of the week.
- Maintain Healthy Weight: Excess body weight places additional pressure on leg veins. A balanced diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats can help achieve and maintain a healthy body mass index.
- Leg Elevation: Elevate your legs above heart level for 15–20 minutes multiple times per day, especially after long periods of standing. This simple practice reduces venous pressure and helps drain fluid from the legs.
- Avoid Prolonged Immobility: If your job involves extended sitting or standing, set a timer to move every 30 minutes. Walk around, do calf raises, or stretch to prevent blood from pooling in your lower legs.
- Wear Supportive Footwear: Choose shoes with low heels and good arch support. Avoid high heels, which limit calf muscle function and impede circulation.
C. Varicose Vein Self-Care
In addition to compression and lifestyle adjustments, consider these self-care techniques:
- Keep Skin Clean and Moisturized: Dry, itchy skin can irritate varicose veins. Use gentle, fragrance-free cleansers and moisturizers to soothe the skin and prevent itching.
- Gentle Massage: Use light upward strokes from ankle to knee to stimulate circulation. Avoid pressing directly on bulging veins. Professional lymphatic drainage massage can further reduce swelling and discomfort.
- Over-the-Counter Pain Relievers: Nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen or naproxen can reduce inflammation and pain. Use as directed and avoid long-term reliance without consulting a healthcare provider.
- Hydration and Nutrition: Stay well hydrated to maintain blood viscosity and prevent vein irritation. Incorporate antioxidant-rich foods (berries, leafy greens) and flavonoid-containing foods (onions, citrus fruits) to strengthen vein walls and reduce inflammation.
VI. Treatment Options for Varicose Veins
A. Overview of Treatment Approaches
Treatment for varicose veins depends on symptom severity, vein size, and individual health factors. Options range from conservative management to minimally invasive procedures and surgical interventions. Goals of treatment include symptom relief, cosmetic improvement, and prevention of complications. A vascular specialist or interventional radiologist can recommend the most appropriate approach based on a thorough evaluation, often including duplex ultrasound to map venous flow.
B. Non-Surgical Treatments
1. Sclerotherapy
Sclerotherapy involves injecting a sclerosant solution—such as polidocanol or sodium tetradecyl sulfate—directly into small to medium varicose veins and spider veins. The solution irritates the vein lining, causing the walls to collapse and seal shut. Over weeks to months, the treated veins are reabsorbed by the body, and blood is rerouted through healthier veins.
- Sessions last 30–60 minutes and may require multiple visits to address all veins.
- Compression stockings are worn for one to two weeks post-procedure to support healing.
- Minor bruising, redness, or itching at injection sites is common and resolves in days to weeks.
2. Endovenous Laser Treatment (EVLT)
Endovenous laser treatment uses laser energy to heat and seal larger varicose veins—commonly the great or small saphenous veins. Under ultrasound guidance, a thin laser fiber is inserted through a tiny puncture in the skin. The laser energy causes the vein wall to collapse and fuse shut. Blood flow then shifts to healthy veins, and the treated vein is absorbed over time.
- Performed under local anesthesia with tumescent solution to numb the area and protect surrounding tissues.
- The procedure takes 45–60 minutes, after which patients can walk and resume light activities immediately.
- Compression stockings are recommended for one to two weeks post-treatment to reduce bruising and promote vein closure.
3. Radiofrequency Ablation (RFA)
Radiofrequency ablation is similar to EVLT but uses radiofrequency energy rather than laser to heat and close the vein. A catheter with a radiofrequency-emitting tip is inserted into the vein under ultrasound guidance. The heat generated by the catheter seals the vein shut. Treated veins are gradually absorbed by the body, and blood flow reroutes to healthy veins.
- The procedure lasts approximately 45 minutes to one hour and is done under local anesthesia with tumescent solution.
- Patients can walk immediately and return to normal activities within a day or two.
- Compression stockings are worn for one to two weeks to support healing and reduce side effects.
4. Foam Sclerotherapy
Foam sclerotherapy is a variation of traditional sclerotherapy in which a foam sclerosant is used. The foam displaces blood within the vein, allowing for better contact with the vein wall. This method is especially effective for larger varicose veins that might not respond as well to liquid sclerosants.
- A fine needle injects the foam directly into the vein under ultrasound guidance.
- Compression stockings are worn post-treatment to ensure vein closure and minimize bruising.
- Multiple sessions may be required depending on vein size and extent.
C. Surgical Treatments
1. Vein Stripping and Ligation
Vein stripping and ligation is a traditional surgical procedure for severe varicose veins. The procedure involves tying off the affected vein at its origin and removing it through small incisions along the leg. Stripping and ligation are typically reserved for cases where minimally invasive methods are not suitable.
- Performed under general or spinal anesthesia, often requiring a short hospital stay or day-surgery setting.
- Recovery time ranges from two to six weeks, with some discomfort and bruising expected.
- Compression stockings and leg elevation aid healing and reduce postoperative swelling.
2. Ambulatory Phlebectomy
Ambulatory phlebectomy—also called microphlebectomy—involves removing visible bulging veins through tiny skin punctures. The procedure is performed under local anesthesia, and stitches are not typically required. It is ideal for veins too large for sclerotherapy but not extensive enough to require stripping.
- Patients can often walk immediately and return to regular activities within a day or two.
- Mild bruising, swelling, or soreness around incision sites may occur but resolves within weeks.
- Compression garments are recommended for one to two weeks post-procedure.
D. Alternative and Complementary Treatments
In addition to conventional medical treatments, some individuals choose alternative approaches to manage varicose vein symptoms. Before trying any complementary therapy, consult with a healthcare professional to ensure safety and avoid interactions:
- Topical Creams and Gels: Over-the-counter products containing horse chestnut extract, witch hazel, or vitamin K claim to reduce swelling and improve vein appearance. While these may provide symptomatic relief, they do not address underlying vein valve dysfunction.
- Herbal Supplements: Horse chestnut extract (aescin), butcher’s broom (ruscogenins), grape seed extract (OPCs), and pycnogenol have venotonic and anti-inflammatory properties. Typical dosages vary: horse chestnut extract 300 mg twice daily, butcher’s broom 150–300 mg daily, grape seed extract 100–300 mg daily, and pycnogenol 50–100 mg daily. Always discuss supplements with your healthcare provider, especially if you take blood thinners or have other medical conditions.
- Acupuncture and Massage Therapy: Acupuncture may improve circulation and reduce leg pain. Gentle massage—particularly lymphatic drainage massage—can decrease swelling and relieve discomfort. Avoid deep tissue massage directly over bulging veins to prevent vein damage.
- Compression Ball Exercises: Rolling a soft ball under the foot or calf can stimulate venous return and ease tension. Perform these exercises for a few minutes several times per day to support muscle pump function.
VII. How to Find Varicose Vein Treatment Near You
When seeking treatment for varicose veins, follow these steps to find a qualified provider:
- Consult Your Primary Care Physician: Your doctor can evaluate your condition, recommend initial conservative measures, and refer you to a vascular surgeon or phlebologist for further evaluation.
- Research Local Vascular Centers: Look for clinics and hospitals with dedicated vascular departments. Review patient testimonials, before-and-after photos, and success rates to gauge quality of care.
- Verify Credentials: Choose board-certified vascular surgeons or interventional radiologists experienced in minimally invasive vein treatments. Ensure they have relevant certifications (e.g., Diplomate of the American Board of Venous and Lymphatic Medicine).
- Check Insurance Coverage: Contact your insurance provider to confirm coverage for varicose vein treatments. Many plans cover medically necessary procedures—such as sclerotherapy for painful veins or EVLT for symptomatic saphenous reflux—when documentation of symptoms and ultrasound findings is provided.
- Schedule a Consultation: During the initial visit, ask about the provider’s experience, approach to treatment, expected outcomes, and potential risks. Request a duplex ultrasound evaluation to map vein reflux and guide a personalized treatment plan.
VIII. When to Worry About Varicose Veins
A. Signs of Serious Complications
While varicose veins themselves often cause discomfort, certain symptoms indicate more urgent issues:
- Skin Changes: New or worsening skin discoloration, thickening (lipodermatosclerosis), or eczema around affected veins suggests chronic venous insufficiency and potential ulceration risk.
- Venous Ulcers: Non-healing sores near the ankles or lower legs that leak fluid or become painful require prompt medical attention to prevent infection and facilitate healing.
- Bleeding: If a varicose vein near the skin’s surface ruptures and bleeds significantly, apply firm pressure and seek immediate care to stop bleeding and address the underlying vein weakness.
- Superficial Thrombophlebitis: Red, tender streaks along a visible vein indicate inflammation and clot formation in a superficial vein. Although less dangerous than deep vein thrombosis, it can cause pain and warrants evaluation.
- Deep Vein Thrombosis (DVT): Symptoms include sudden, intense leg pain, significant swelling, warmth, and redness—often in the calf or thigh. DVT is a medical emergency, as a clot can break off and travel to the lungs, causing a pulmonary embolism. Seek emergency care immediately.
B. When to Consult a Specialist
If you experience any of the above complications or if varicose vein symptoms—pain, swelling, skin changes—persist despite conservative care, schedule an appointment with a vascular specialist. Early intervention can prevent further progression, reduce complication risk, and improve treatment outcomes.
IX. Frequently Asked Questions
A. Can varicose veins go away on their own?
While some mild varicose veins may improve after pregnancy or weight loss, they generally do not disappear without treatment. Conservative measures—such as compression stockings, exercise, and leg elevation—can reduce symptoms and slow progression, but medical or procedural interventions are often needed to eliminate visible veins.
B. Are varicose veins dangerous?
In most cases, varicose veins are not life-threatening. However, if left untreated, they can lead to complications such as skin ulcers, venous eczema, superficial thrombophlebitis, or deep vein thrombosis. These complications can cause pain, infection, and more serious health issues. Monitoring symptoms and seeking timely evaluation can prevent dangerous outcomes.
C. Are there natural ways to prevent varicose veins?
While genetics and age play significant roles, you can reduce your risk by:
- Maintaining a healthy weight to lessen pressure on leg veins.
- Exercising regularly—especially walking, cycling, or swimming—to strengthen calf muscles.
- Avoiding prolonged sitting or standing; take breaks to move every 30 minutes.
- Wearing compression stockings during high-risk activities (long flights or standing job shifts).
- Elevating legs above heart level for 15–20 minutes multiple times per day to reduce venous pressure.
D. Can varicose veins affect pregnancy and fertility?
Varicose veins often develop or worsen during pregnancy due to increased blood volume and hormonal changes. They generally improve postpartum, but some may persist. Testicular varicoceles can affect male fertility by impairing sperm production and function. If you have fertility concerns, consult a specialist for evaluation and possible treatment.
E. How long does recovery take after varicose vein procedures?
Recovery varies by procedure type:
- Sclerotherapy and Foam Sclerotherapy: Minimal downtime; most people resume normal activities immediately, with compression stockings worn for one to two weeks.
- EVLT and RFA: Walk immediately post-procedure; return to light activities the same day. Compression stockings for one to two weeks; full recovery in 1–2 weeks.
- Microphlebectomy: Minimal downtime; walk immediately; compression stockings for one to two weeks; minor bruising may last a few weeks.
- Vein Stripping and Ligation: Several weeks of recovery; walking encouraged early; compression stockings and leg elevation recommended; full return to strenuous activity in 4–6 weeks.
X. Conclusion
Varicose veins are a common vascular condition that can cause pain, discomfort, and aesthetic concerns. By understanding their causes—such as valve dysfunction, venous hypertension, and contributing risk factors like genetics and lifestyle—you can take early steps to prevent or manage the condition. Conservative measures including compression therapy, exercise, leg elevation, and healthy weight maintenance often provide significant symptom relief. When these methods are insufficient, minimally invasive procedures (sclerotherapy, EVLT, RFA, microphlebectomy) offer rapid, effective results with minimal downtime. In advanced cases, surgical interventions may be necessary. Prevention and long-term management involve regular exercise, maintaining a healthy weight, avoiding prolonged immobility, and wearing compression stockings during high-risk situations. If you experience persistent pain, skin changes, or signs of complications, consult a vascular specialist for personalized evaluation and treatment. Proactive care can improve quality of life, reduce discomfort, and maintain healthier veins for years to come.
Disclaimer: This article is intended for informational purposes only and does not constitute medical advice, diagnosis, or treatment. The content provided should not be used as a substitute for professional medical advice, diagnosis, or treatment. Always consult with a qualified healthcare professional before making any decisions about your health or medical conditions. Never disregard or delay seeking professional medical advice due to the information provided in this article. The author and publisher of this article are not responsible or liable for any adverse outcomes resulting from the use or reliance on the information provided herein.